Hip Replacement
Contact Us
Request an AppointmentPlease note that a referral letter is required before an appointment can be confirmed.
Please note that a referral letter is required before an appointment can be confirmed.
Useful Information
About this service
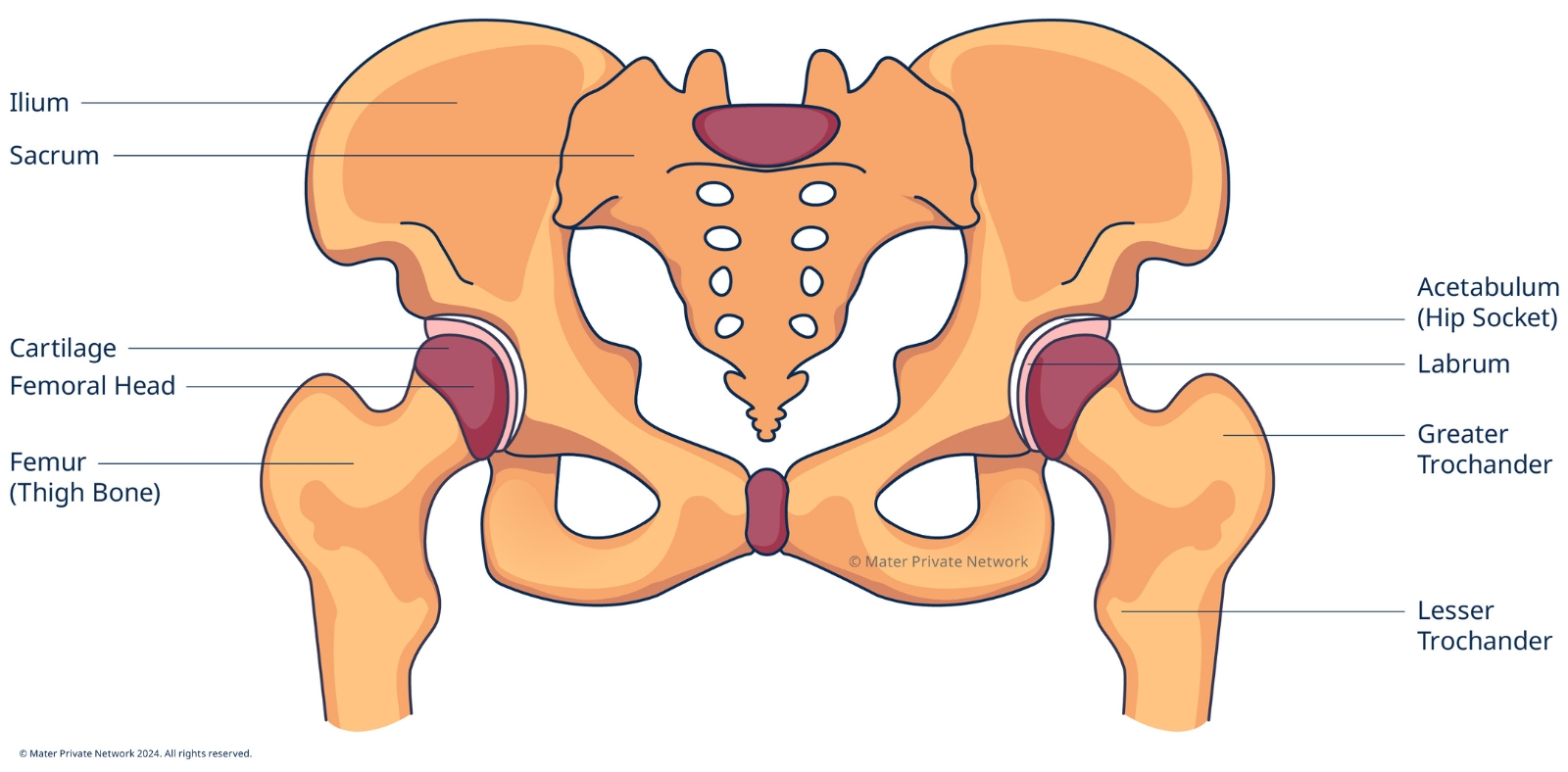
Hip replacement surgery involves removing a painful hip joint and replacing it with a new artificial joint usually made from metal and plastic components. A hip replacement may be recommended if your hip joint is worn or damaged, leading to reduced mobility and pain. Joint degradation may be caused by degenerative disorders such as osteoarthritis, rheumatoid arthritis, or injuries to the joint.
The surgery helps thousands of people each year to relieve pain and resume mobility. It is acknowledged as one of the most consistently successful and life-changing operations performed today.
Common causes of hip pain
The most common causes of chronic hip pain include:
- Osteoarthritis is the most common type of arthritis and occurs when the cartilage and other tissues within the joint break down, which usually happens gradually over time. Certain factors may make it more likely for you to develop osteoarthritis such as ageing, a history of trauma or injury to the joint, and family history of osteoarthritis.
- Rheumatoid arthritis is caused by an autoimmune disorder, where the body’s immune system mistakenly attacks the body’s healthy tissue affecting the lining of the joints.
- Post-traumatic arthritis can develop after an injury to the joint, leading to accelerated wear and tear of the cartilage over time.
- Hip dysplasia causes the hip socket to be abnormally shallow, causing the bone of the femur to not fit securely into the socket.
Pre-operative assessment clinic
Within a month of your operation, you may be invited to attend the pre-operative assessment clinic. During this visit you will be asked about your medical history and any medications you are taking. Blood tests will be carried out and you may have an ECG and x-ray.
Pain management plays an important part in recovery and rehabilitation and is often of great concern for patients. The consultant anaesthetist and nurse at the clinic will talk to you about pain management after surgery.
The pre-operative assessment clinic gives you the opportunity to see the physiotherapist and nurse, ask any questions you may have and plan for your discharge from hospital.
You and your the healthcare team will work together to carry out several actions before and after surgery to reduce the risks of complications. It is important to be in the best possible overall health and there are a number of things you can do to prepare for surgery, recovery and rehabilitation.
- Diet: in the weeks before surgery eat a balanced diet as this can help the healing process.
- Smoking: smoking may cause complications with anesthesia and nicotine can delay or interfere with healing. In both cases, this can affect the outcome of the surgery. If you are able to give up or reduce smoking as far in advance as possible before the surgery, this would aid your recovery. Even one week of no smoking would still be helpful.
- Blood clots: to reduce the risk of developing a blood clot in the legs or lungs, a number of recommendations will be given in advance of your surgery.
- Infection: if there are any signs or symptoms of an infection, such as a chest or urinary infection in the days prior to surgery, inform the surgeon. The surgeon will also need to be advised of rash or flare up of psoriasis or eczema around the hip area or a leg ulcer. If you have a history of MRSA/VRE or have been in contact with someone with MRSA/VRE, you should inform your healthcare team.
- Exercise: it is important to be as fit as possible before the procedure, as this will make recovery much faster. You will be given a personal exercise programme to follow in advance of and for a time after the procedure.
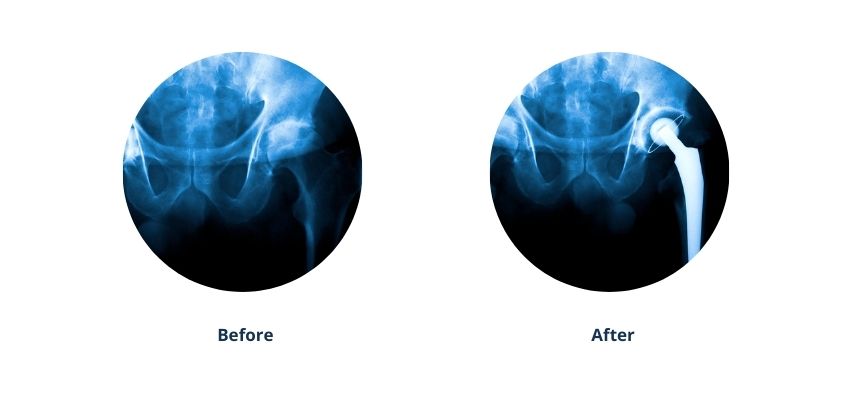
Any damaged cartilage and bone will be removed and the hip joint will be replaced with an implant. A total hip replacement procedure takes a few hours. The surgeon will select the type of implant that best suits a patient's needs.
Hip replacement surgery is generally carried out under spinal anaesthetic with sedation. A consultant anaesthetist will discuss anaesthetic options with you, as well as the risks and benefits associated with each.
You will be held in the recovery area until you are stable enough to return to the ward where the team will work closely to aid recovery.
You will have a drip for intravenous fluids through a vein into the arm or hand which will continue until you are able to eat and drink again. You may eat and drink as required, commencing with sips of water followed by a light meal.
A drip may be inserted in the hip which is normally removed one to two days after surgery.
Your discharge date will be determined by all members of the healthcare team involved in your care, who will work in consultation with your family.
Discharge from hospital normally occurs when you reach specific goals such as the distance you can walk or how much your wound has healed. The surgeon will discuss the expected length of stay prior to admission.
Following discharge, you will continue your recovery at home in your own familiar environment. You will be given a home exercise programme and you can book in for outpatient physiotherapy if required or advised by your surgeon.
Hip Replacement Physio Programme: Weeks 0-6 following surgery
Hip Replacement Physio Programme: Weeks 7-12 following surgery
Frequently asked questions
You will initially walk with a frame and staff assistance, over time progressing to walking with two walking sticks or elbow crutches. The physiotherapy team will guide you on the journey to walk independently with the appropriate mobility aid. Our shared goal is to have you walking independently before you leave the hospital.










/mr.-james-cashman-.png?sfvrsn=806f0b0_1)
/john-gibbons-(240-x-240).jpg?sfvrsn=bcc09834_1)
/mr.-mike-leonard-.png?sfvrsn=adc24a07_1)

/kevin-mulhall-(240-x-240).jpg?sfvrsn=4c34c37e_1)
/mr.-martin-murphy.jpg?sfvrsn=2675ece9_1)
/mr.-keith-synnott.jpg?sfvrsn=8ba22a95_1)
/mr.-nikolas-davarinos.png?sfvrsn=687dd18e_1)
/adeel-memon-2024-(240-x-240).jpg?sfvrsn=1df9412c_1)
/mr.-padhraig-o'loughlin-.jpg?sfvrsn=832fd6fc_1)
