Endoscopic Retrograde Cholangiopancreatography (ERCP)
Contact Us
Request an AppointmentPlease note that a referral letter is required before an appointment can be confirmed.
Useful Information
About Endoscopic Retrograde Cholangiopancreatography (ERCP)
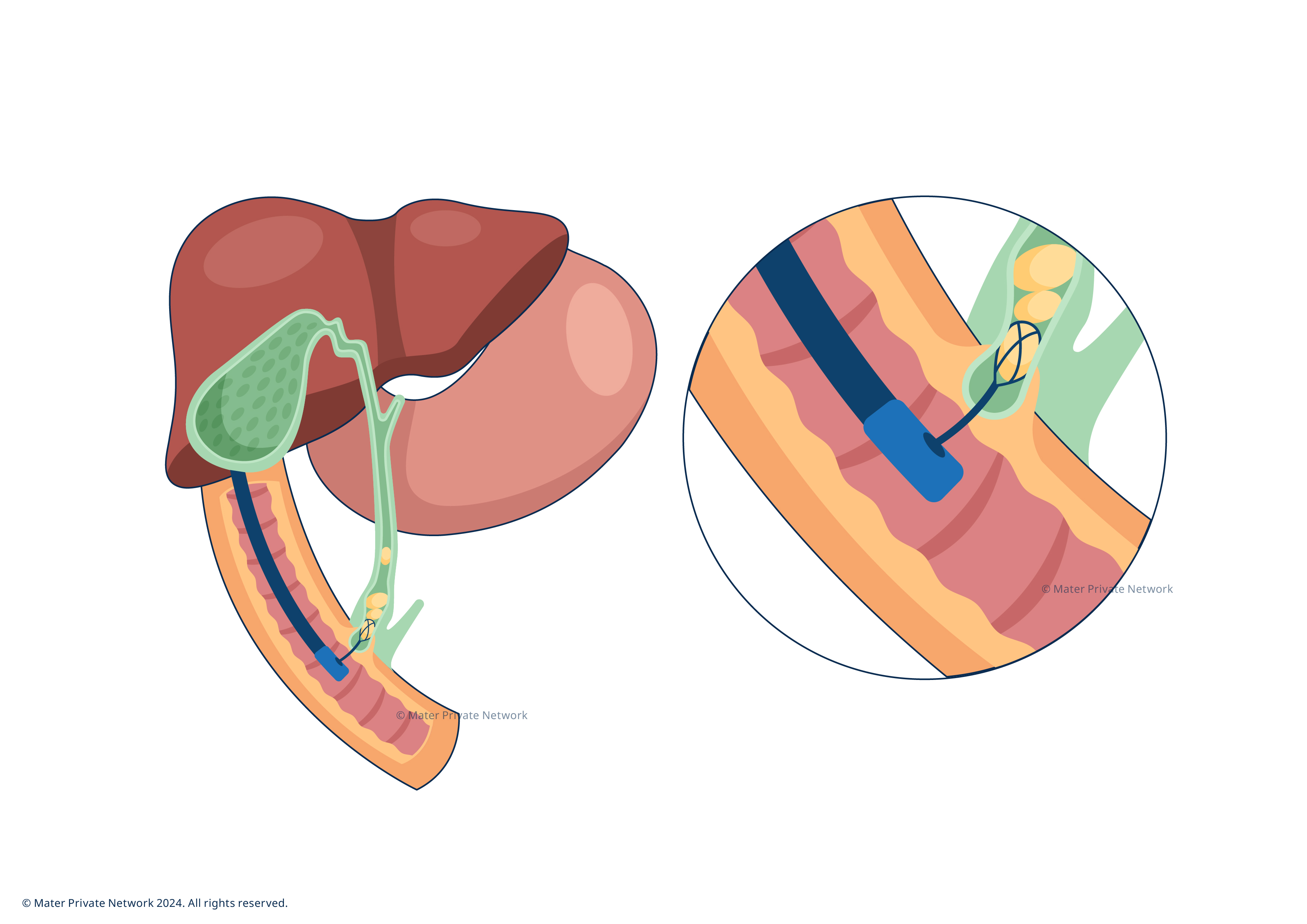
Endoscopic Retrograde Cholangiopancreatography (ERCP) is a procedure used mainly to diagnose and treat diseases affecting the bile ducts. Bile ducts are tiny canals that carry bile between the liver, the gallbladder, and the small intestine to aid digestion. ERCP is particularly useful for removing bile duct stones, inserting stents to open blockages, and taking tissue samples for further analysis.
ERCP uses endoscopy (a procedure where a thin tube with a camera, called a scope, is used to examine areas inside your body) and fluoroscopy (an imaging procedure that uses several pulses of an X-ray beam to take real-time footage inside your body) together to examine the ducts and carry out procedures.
Why do I need an ERCP?
Your doctor may have referred you for an ERCP for any of the following conditions:
- Bile Duct Stones: to remove stones that are causing blockages or infections.
- Pancreatitis: to diagnose and treat the causes of inflammation in the pancreas.
- Bile Duct Strictures: to widen narrowed areas and make sure that your bile (digestive fluid produced in your liver and stored in your gallbladder) is able to travel to your intestine.
- Jaundice: to identify and address blockages that are causing yellowing of the skin and eyes.
- Tumours or Cancers: to diagnose and treat cancers of the bile ducts, pancreas, or gallbladder.
What are the benefits of ERCP?
The benefits of ERCP include:
- Precise diagnosis: this procedure provides a detailed view of the bile and pancreatic ducts, allowing for accurate diagnosis of conditions such as blockages, strictures, and tumours.
- Direct visualisation: ERCP enables direct visualisation of the bile ducts, pancreas, and gallbladder, which can be more informative than other imaging techniques like MRI or CT scans.
- Immediate treatment: ERCP not only diagnoses problems but also allows for immediate treatment, such as removing bile duct stones or placing stents to relieve blockages.
- Targeted approach: the ability to directly target the area of concern allows for more precise treatment, reducing the need for multiple procedures.
- Minimally invasive: compared to surgical alternatives, ERCP is less invasive, often resulting in shorter recovery times and reduced hospital stays.
- Quick recovery: most patients can return to normal activities within a day or two.
What to expect when having an ERCP
Preparation: Your consultant will discuss the procedure with you. You will need to fast for at least 6 hours before the procedure to ensure your stomach is empty. If you are taking any medications, particularly blood thinners, please discuss this with your consultant before you make your ERCP appointment.
If you have the procedure as an outpatient, you might need a recent blood test, including a blood clotting test, which your GP can do for you.
Arrival: On the day of the procedure, you should come to the Endoscopy unit where you will be admitted by our administration team. Please bring with you a list of any medications you are taking. One of our nursing team will meet you and take initial readings of your blood pressure heart rate and your oxygen saturations. You will then be brought into the Endoscopy Room where your consultant will discuss your medical history and symptoms with you.
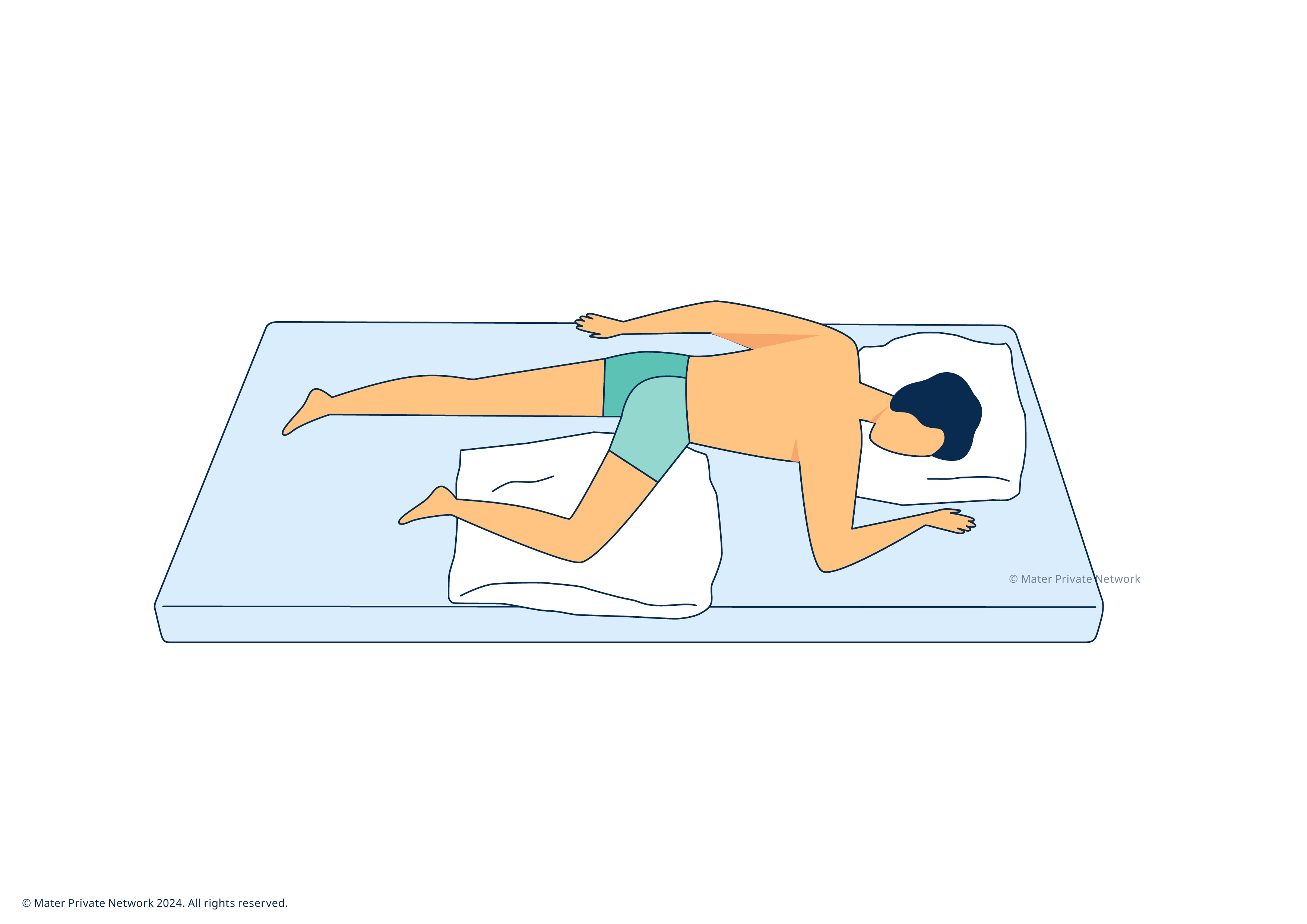
You will be given a numbing spray in your throat. You will then be asked to lie on your left side with your mouth facing towards your right shoulder. Once you are in the correct position, a mouthpiece will be placed to protect your teeth/gums. You will then be given pain relief medication and a ‘conscious’ sedative, which means that you will be awake during the procedure but won’t feel anything and or be able to speak.
When you are ready, your consultant will pass a tube with a camera through your mouth, down to the small bowel called duodenum in order to access the common bile duct. Your consultant will use the camera to assess the area and depending on your needs, will carry out the necessary procedure whether this is removing stones, taking tissue samples or inserting a stent. The procedure can take between 20 minutes to 1 hour depending on each case.
You will be monitored as the sedation wears off. Your consultant will discuss the results and any next steps with you once you’re awake; if you are having the procedure as an outpatient, you will be able to go home as soon as you feel ready.
Your consultant will advise when to restart blood thinning medications. You should continue to fast for 2 hours after the procedure. After that, you should then take only a liquid diet for the following 12 hours (soup, jelly, ice cream, tea, juices). You can then eat normally again. You might feel discomfort in your throat, but this should improve over the next 6-12 hours, and you can use regular pain relief to help.
The nurse will discuss all the relevant discharge information and give you a direct hospital contact number in the event of any questions or complications.
The consultant may arrange a follow up procedure or clinic review if needed.
ERCP is generally safe but comes with some risks, including:
- Post ERCP Pancreatitis (PEP): slight risk (1in 20) of swelling that causes abdominal pain. In such a case, you will be kept in hospital for 1-2 days for treatment. In rare cases, pancreatitis can require surgery or admission to the ICU.
- Internal bleeding (Sphincterotomy bleed): risk is slight (1 in 30) and can occur 24-48 hours after the procedure (delayed bleeding). Generally, any bleeding is minor and settles itself, but further treatment might be necessary.
- Perforation: the risk of perforation (a tear) during ERCP is 1 in 50-100. If this occurs, you may have to stay in the hospital for a number of days and will be treated with antibiotics, painkillers and intravenous fluids. In rare cases surgery may be needed.
- Medication-related side effects: the sedative medications used can sometimes lower your blood pressure, heart rate or oxygenation levels. Rarely, people have an allergic reaction to the numbing spray. If any of these side-effects occur, you will be treated in the hospital. Please inform a member of your healthcare team of any allergies (including contrast dye which will be used to take pictures of bile ducts with X-ray machine).
- Infection: slight risk (up to 1 in 30). This is usually treated with antibiotics.
- Missed diagnosis: there is a rare chance that small stones or strictures may be missed.
- Failure of the procedure: If this happens (1 in 20), alternate treatments will be discussed with you after the procedure. In some cases, a second attempt at ERCP to clearing the duct may be required.
- X-Ray exposure: this procedure includes exposure to X-rays. If relevant, you will be asked to confirm that you are not pregnant prior to the procedure.
Frequently Asked Questions
ERCP is an advanced form of endoscopy that uses an extension to reach beyond your upper GI tract to access your biliary ducts. This extension allows your consultant to operate directly on your bile ducts. ERCP is the only endoscopic procedure that allows this.
The specific purpose of ERCP is to visualise and treat the bile ducts and pancreas, while endoscopy examines only the lining of stomach.
While endoscopy relies on a camera attached to a flexible tube, ERCP combines this with imaging technology to highlight the flow of bile.
The procedure can take between 20 minutes to an hour, depending on the complexity of the case.
You will be sedated, which means you will be awake but very relaxed and generally won’t remember much of the procedure.
Most people can return to normal activities within a day or two but strenuous activities should be avoided for a few days.
Depending on your condition, the procedure can be carried out as an outpatient or an inpatient. If the former, you will usually be able to go home after the procedure. However, this decision lies with consultant and depends on many factors which will be discussed with you.







.jpg?sfvrsn=1dfe5454_1)


/rahim-khan-(240-x-240).jpg?sfvrsn=7249a2e5_1)
